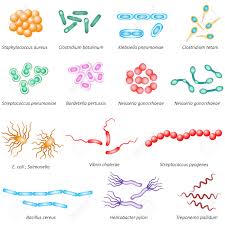
Disease and decay are not inherent properties of organic objects, nor are they caused by physical damage, it is microorganisms that bring about these changes. We are surrounded by bacteria, virus, and fungi. Many cause diseases in cattle and crops and others are known for entering human bodies and causing various diseases.
Examples of familiar human diseases are:
Bacteria: pneumonia, bacterial dysentery, diphtheria, bubonic plague, meningitis, typhoid, cholera, salmonella, meningococcal
Virus: Chickenpox, measles, mumps, German measles, colds, warts, cold sores, influenza
Protoctista: amoebic dysentery, malaria,
Fungi: ringworm, athlete’s foot
Diseases – Communicable diseases, Endemic diseases
Top 10 Causes of Death (Source: WHO World Health Statistics 2012)
- Ischemic heart disease 12 %
- Chronic obstructive pulmonary disease 11%
- Stroke 9%
- Diarrheal disease 6%
- Lower respiratory infections 5%
- Preterm birth complications 4%
- Tuberculosis 3%
- Self-inflicted injuries 3%
- Falls 3%
- Road injuries 2%
Communicable diseases
- Communicable diseases continue to be a major public health problem in India.
- Many communicable diseases like tuberculosis, leprosy, vector borne diseases like malaria, kalaazar, dengue fever, chikungunya, filariasis, Japanese encephalitis, water-borne diseases like cholera, diarrhoeal diseases, viral hepatitis A & E, typhoid fever, leptospirosis, etc and other viral infections are endemic in the country.
- In addition to these endemic diseases, there is always a threat of new emerging and re-emerging infectious diseases like nipah virus, avian influenza, SARS, novel H1N1 influenza, hanta virus etc.
- Local or widespread outbreaks of these diseases result in high morbidity, mortality and adverse socio-economic impact.
The most common diseases which are endemic in India are as follows:
Communicable Disease- Malaria:
- Malaria is a very common disease in developing countries. The word malaria is derived from the word ‘mal-aria meaning bad air.
- Ronald Ross first discovered the transmission of malaria by mosquitoes, while he was working in India (Secunderabad, AP) in 1897. Malaria is one of the most widespread diseases in the world.
- Each year, there are 300 to 500 million clinical cases of malaria, 90 percent of them in Africa alone.
- Among all infectious diseases, malaria continues to be one of the biggest contributors to disease burden in terms of deaths and suffering.
- Malaria kills more than one million children a year in the developing world, accounting for about half of malaria deaths globally.
- The risk of getting malaria extends to almost the entire population in India (almost 95 percent).
- The following states that have the highest number of malaria cases are Madhya Pradesh, Maharashtra, Orissa, Karnataka, Rajasthan, Assam, Gujarat and Andhra Pradesh.
Communicable Disease- Typhoid:
- Typhoid fever is an acute, systemic infection presenting as fever with abdominal symptoms, caused by Salmonella typhi and paratyphi.
- Before nineteenth century, typhus and typhoid fever were considered to be the same. Enteric fever is an alternative name for typhoid. Salmonella typhi and paratyphi colonise only humans.
- The organisms are acquired via ingestion of food or water, contaminated with human excreta from infected persons.
- Direct person-to-person transmission is rare. Typhoid is a global health problem. It is seen in children older than the age of one.
- Outbreak of typhoid in developing countries results in high mortality. The recent development of antibiotic resistant organisms is causing much concern.
- Typhoid fever is more common in the tropics. It tends to occur in places, where the sanitation standards are poor. A bacterial organism called salmonella typhi causes typhoid fever.
- Salmonella paratyphi can also cause fever and abdominal symptoms. The disease caused by both these entities is called enteric fever.
- The disease presents with a typical, continuous fever for about three to four weeks, relative bradycardia with abdominal pain (due to enlargement of lymph nodes in the abdomen), and constipation.
- Geographical Distribution Worldwide, typhoid fever affects about six million people with more than 6, 00,000 deaths a year.
- Almost 80 percent of cases and deaths occur in Asia, and most others in Africa and Latin America. Among Asian countries, India probably has a large number of these cases.
- Indian Statistics Typhoid fever is endemic in India.
- Health surveys conducted by the Central Ministry of Health in the community development areas indicated a morbidity rate varying from 102 to 2,219 per 1, 00,000 population in different parts of the country.
- A limited study in an urban slum showed 1 percent of children up to 17 years of age suffer from typhoid fever every year.
- Carriers of Typhoid Fever Typhoid infection is mainly acquired from persons who are carriers of the disease.
- Carriers are the people who continue to excrete salmonella through their urine and feces a year after an attack of typhoid. A chronic carrier state develops in about 2 to 5 percent of the cases.
- The organisms in such cases make the gall bladder their habitat.
Communicable Disease- Hepatitis:
- Hepatitis is the inflammation of liver. It can be caused by viruses (five different viruses— termed A, B, C, D and E cause viral Hepatitis), bacterial infections, or continuous exposure to alcohol, drugs, or toxic chemicals, such as those found in aerosol sprays and paint thinners, or as a result, of an auto-immune disorder.
- Hepatitis results in either damage or reduction in the livers ability to perform life-preserving functions, including filtering harmful, infectious agents from blood, storing blood sugar and converting it into usable energy forms, and producing many proteins necessary for life.
- Symptoms seen in Hepatitis differ according to the cause and the overall health of the infected individual. However, at times, the symptoms can be very mild.
- The commonly seen clinical features are general weakness and fatigue, loss of appetite, nausea, fever, abdominal pain and tenderness.
- The main feature is the presence of jaundice (yellowing of skin and eyes that occurs when the liver fails to break-down excess yellow- coloured bile pigments in the blood).
- Depending on the progress and intensity, Hepatitis can be categorized as acute or chronic. In acute Hepatitis, clinical features often subside without treatment within a few weeks or months. However, about 5 percent of the cases go on to develop into chronic Hepatitis, which may last for years. Chronic Hepatitis slowly leads to progressive liver damage and cirrhosis.
Hepatitis A:
- Hepatitis A is a self-limiting disease that is found all across the world.
- It is usually transmitted through oral ingestion of infected material (mainly water), but sometimes transmitted parenterally; most cases resemble the symptoms of a mild flu attack and jaundice is mild too.
Hepatitis B:
- Hepatitis B is an acute vital disease. It primarily spreads parenterally, but sometimes orally as well.
- However, the main mode of spread is intimate contact and from mother to the new born.
- Fever, anorexia, nausea, vomiting are the initial symptoms, and they soon lead to severe jaundice, urticarial skin lesions, arthritis, etc.
- Some patients become carriers or even remain chronically ill, even though most patients recover in about three to four months.
Hepatitis C:
- Hepatitis C is a viral disease commonly occurring after transfusion or parenteral drug abuse.
- It frequently progresses to a chronic form that is usually asymptomatic, but may involve liver cirrhosis.
Hepatitis D:
- Hepatitis D or Delta Hepatitis is caused by the Hepatitis D virus.
- It usually occurs simultaneously with or as a super infection in case of Hepatitis B, thus increasing its severity.
Hepatitis E:
- Hepatitis E is transmitted by the oral fecal route; usually by contaminated water.
- Chronic infection does not occur but acute infection may be fatal in pregnant women.
Communicable Disease- Jaundice:
- Jaundice, also known as icterus, is a condition, which is characterized by yellowish discolouration of the skin and whites of eyes. It is a symptom or clinical sign, not a disease by itself.
- The yellow colouration is caused by an excess amount of bile pigment known as bilirubin in the body. Normally, bilirubin is formed by the breakdown of haemoglobin during the destruction of worn-out red blood cells.
Communicable Disease- Leptospirosis:
- Leptospirosis is a disease caused by a type of bacteria and is associated with animals. It is more common in the tropical countries.
- The disease is also known as canefield fever; cani- cola fever, field-fever, mud fever, seven day fever and swineherd disease. Leptospirosis is caused by different strains of bacteria of the genus Leptospira.
- Of all the varieties that cause disease, Leptospira icterohaemorrhagiae is the most serious type.
- If not treated properly, it could lead to serious complications. Leptospirosis is a disease of animals that can spread to humans.
- Rats are the most common carriers. Soil contaminated with urine of infected animals can also transmit the disease to persons exposed to cattle urine, rat urine or to foetal fluids from cattle.
- Sewage workers, agricultural workers, butchers, meat inspectors, workers in contact with contaminated waters and veterinarians are generally at risk.
- Person to person transmission is not possible. Leptospirosis can spread due to contact with urine, blood or tissues from infected persons. The organisms enter the body through the breaks in the skin or through mucous membranes.
- The organisms can also be acquired by drinking contaminated water. Infection is commonly acquired by bathing in contaminated water.
- The organisms multiply in the blood and tissues of the body. Though the organism can affect any organ of the body, the kidney and liver are commonly involved. The incubation period is usually 10 days. It may vary from 2 to 20 days.
Communicable Disease- Diarrhoeal Diseases:
- The term gastroenteritis’ is most frequently used to describe acute diarrhoea. Diarrhoea is defined as the passage of loose, liquid or watery stools.
- These liquid stools are usually passed more than three times a day. The attack usually lasts for about 3 to 7 days, but may also last up to 10 to 14 days.
- Diarrhoea is a major public health problem in developing countries. Diarrhoeal diseases cause a heavy economic burden on health services.
- About 15 percent of all pediatric beds in India are occupied by admissions due to gastroenteritis.
- In India, diarrhoeal diseases are a major public health problem among children under the age of 5 years. In health institutions, up to a third of total pediatric admissions are due to diarrhoeal diseases.
- Diarrhoea related diseases are a significant cause of mortality in children less than five years of age. Incidence is highest in the age group of 6 to 11 months.
- The National Diarrhoeal Disease Control Programme has made a significant contribution in averting deaths among children less than five years of age.
Communicable Disease- Amoebiasis:
- Amoebiasis is an infection caused by a parasite ‘Entamoeba Histolytica. The intestinal disease varies from mild abdominal discomfort and diarrhoea to acute fulminating dysentery.
- Extra intestinal amoebiasis includes involvement of the liver (liver abseess), lungs, brain, spleen, skin, etc.
- Amoebiasis is a common infection of the human gastrointestinal tract. It has a worldwide distribution.
- It is a major health problem in the whole of China south-east and west Asia and Latin America, especially Mexico. It is generally agreed that amoebiasis affects about 15 percent of the Indian population. Amoebiasis has been reported throughout India.
Communicable Disease- Cholera:
- Cholera is an acute diarrhoeal disease caused by V. Cholera (classical or El T). It is now commonly due to the El T or biotype.
- The majority of infections are mild or symptomatic. Epidemics of cholera are characteristically abrupt and often create an acute public health problem.
- They have a high potential to spread fast and cause deaths. The epidemic reaches a peak and subsides gradually as the ‘force of infection declines.
- Often, when time control measures are instituted, the epidemic has already reached its peak and is waning.
Communicable Disease- Brucellosis:
- Brucellosis is one of the major bacterial zoonoses, and in humans is also known as undulent fever, Malta fever or Mediterranean fever.
- It is occasionally transmitted to humans by direct or indirect contact with infected animals.
- The disease may last for several days, months or occasionally, even years.
- Brucellosis is both a severe human disease and a disease of animals with serious economic consequences. Brucellosis is a recognized public health hazard that is found the world over.
- It is endemic wherever cattle, pigs, goats and sheep are raised in large numbers. The important endemic areas for Brucellosis exist in Mediterranean zones, Europe, Central Asia, Mexico and South America. Animal Brucellosis has been reported from practically every state in India.
- However, no statistical information is available about the extent of infection in humans in various parts of the country.
- The prevalence of human Brucellosis is difficult to estimate. Many cases remain undiagnosed either because they are not apparent, or because physicians in many countries are unfamiliar with the disease.
Communicable Disease- Hookworm Infection:
- Hookworm infection is defined as: ‘any infection caused by Ancylostoma or Necator’.
- They may occur as single or mixed infections in the same person through various factors, which have to be prevented. Hookworm infection is widely prevalent in India.
- Necator americanus is predominant in south India, and Ancylostoms duodenal in north India. Recently, another species, A. ceylanicum has been reported from a village near Calcutta.
- The heavily infected areas are found in Assam (tea gardens).
- West Bengal, Bihar, Orissa, Andhra Pradesh, Tamil Nadu, Kerala and Maharashtra. More than 200 million people are estimated to be infected in India.
- It is believed that 60 to 80 percent of the population of certain areas of West Bengal, Uttar Pradesh, Bihar, Orissa, Punjab, and the eastern coast of Tamil Nadu and Andhra Pradesh are infected with hookworms.
Communicable Disease- Influenza:
- Influenza is an acute respiratory tract infection caused by influenza virus of which there are three types—A, B and C.
- All known pandemics were caused by influenza A strains, due to various factors. Influenza is found all over the world.
- It occurs in all countries and affects millions of people. Outbreaks of influenza A occur virtually every year. Major epidemics occur at intervals of two to three years, and pandemics at intervals of about 10 to 15 years.
- The first pandemic during the present century occurred in 1918-19, which affected an estimated 500 million people and killed more than 20 million.
- In India alone, over six million people died during this pandemic. This pandemic was caused by what is now known as the swine influenza virus.
- Recent pandemics occurred in 1957-58 owing to the influenza A (H2N2) and in 1968 owing to the influenza A (H3N2).
- Outbreaks of influenza B also occur annually with epidemics occurring at intervals of407 years. Influenza brought on by the type C virus occurs sporadically as small outbreaks.
- The unique features of influenza epidemics are the suddenness with which they arise, and the speed and ease with which they spread.
- The short incubation period, a large number of subclinical cases, a high proportion of susceptible population, short duration of immunity, and an absence of cross-immunity, all contribute to its rapid spread.
- The fate of the virus during inter-epidemic periods is also known. Possible explanations include transmission of virus to extra-human reservoirs (pigs, horses, birds. etc.,) latent infection or continuous transfer from one human to another. This explains the occurrence of sporadic cases.
Communicable Disease- Filariasis:
- It is caused by a parasite, which belongs to the nematode family Filariasis. According to WHO reports, an estimated 751 million people are at ‘risk’ for infection, and 120 million have actually been infected.
- The public health problem of lymphatic filariasis is greatest in China, India and Indonesia. These three countries account for about two-thirds of the estimated world total of persons infected.
Filarial Problem in India:
- Filariasis is a major public health problem in India. There are an estimated six million attacks of acute filarial disease per year, and at least 45 million persons currently have one or more chronic filarial lesions.
- Heavily infected areas are found in Uttar Pradesh, Bihar, Andhra Pradesh, Orissa, Tamil Nadu, Kerala and Gujarat.
- The infection is acquired from a person who has filariasis. The maximum infectivity is when the organisms are circulating the blood.
- The largest number appears in the blood at night time, and retreats from the blood stream during the day. Their usual habitat is in the lymph nodes.
- The mosquito feeds on such a person and acquires the filarial parasite. The filarial organism is transmitted when the mosquito bites a person. The parasite is deposited near the site of puncture.
- It passes through the punctured skin or may penetrate the skin on its own and finally reach the lymphatic system. Filariasis affects all age groups.
Communicable Disease- Tuberculosis:
- Tuberculosis remains a worldwide public health problem, particularly in the Third World countries. Tuberculosis is India’s biggest public health problem. An estimated that 5, 00,000 deaths annually are reported due to this disease, while a similar number of persons get cured.
- The population in the Third World countries like India is exposed to tuberculosis. The disease, however, does not develop in everyone who is exposed. Poor nutrition, overcrowding, low socio-economic status, are more likely to develop the disease.
- The prevalence of people who are infected is about 30 percent of the population. The prevalence of infection is more common in the younger population.
- The vast majority of cases are to be found in rural and semi-urban areas, where more than 80 percent of the country’s population lives. In urban areas, tuberculosis is found more frequently in slum-dwellers and lower socio-economic groups than in well-off groups
Current Burden of Non-Communicable Diseases in India
- Non communicable diseases are the one which are of long duration and slow in progression. As per World health organization, NCDs account for total 53% of all deaths in India. Most of the burden is attributed by cardiovascular diseases (24%), followed by respiratory diseases (11%), other NCDs (10%) and Injuries (10%).
- According to a report presented by world economic forum and Harward School of public health, the prevalent NCDs in India are CVDs, chronic respiratory diseases, Diabetes, and cancer.
- Cancer is one the leading cause of death in India with 28 lac cases at a point of time and 10 lac new cases taking place very year. The burden of cancer is expected to rise in the country due to the effects of tobacco, demographic transitions and increase in the life expectancy.
- Diabetes is another leading NCD in the nation. Estimated total number of people suffering with diabetes is 40.9 million in India and by 2025 it is expected to increase up-to 69.9 million. Diabetes accounts for 1.09 lakh deaths in a year.
- Hypertension is a major risk factor for cardiovascular diseases. Hypertension is directly responsible for 57% of all stroke deaths and 24% of all coronary heart disease deaths in India. The cases of CVDs are expected to rise up to 741 lacs in 2015.
- Chronic obstructive pulmonary disease is responsible for high rate of mortality and morbidity across the world. In 2010, almost 24 million adults over the age of 40 in India had COPD. It is expected to increase to 32 million by 2020.
- The other conditions which contribute to the burden of non-communicable diseases are mental health conditions (schizophrenia, depression & bipolar disorder) and musculoskeletal disorders (Rheumatoid arthritis, osteoarthritis & gout).
- The non-communicable diseases are emerging due to the risk factors associated with it. The main risk factors which are associated with NCDs are tobacco use, harmful use of alcohol, lack of physical activity and poor diet.3Table 2&3 shows the risk factors(Behavioral & Metabolic respectively) associated with noncommunicable diseases and their prevalence.
- In addition to the above said risk factors for NCDs; Globalization and urbanization has also contributed to its burden. It has caused the nutritional transition in the country because of the availability of the commercial food. One another important factor causing the rise in NCDs is change in demographic profile of the country.
- A study conducted by Joy Kumar Chakma & Sanjay Gupta on“Lifestyle and Non-Communicable Diseases: A double edged sword for future India” showed that In India, 53% of the deaths in 2008 were due to NCDs (WHO). The cardiovascular diseases (CVDs) alone account for 24 percent of all deaths.
- The anticipated cumulative loss of national income due to NCDs mortality for India for 2006-2015 will be USD237 billion. By 2030, this productivity loss is expected to double. These major NCDs can be prevented through effective interventions by undertaking the lifestyle related modifiable risk factors.
- Total deaths (in thousands) caused by non-communicable diseases as per WHO (2008) estimates are 2967.6 and 2273.8 among males and females respectively. NCD deaths under the age of 60 years are 35.0% (Males) and 32.1% (Females).
Epidemic diseases
Complete information on major types of epidemics in India
- India is endemic to many diseases such as Malaria, Kala-azar, Cholera, Tuberculosis. These erupt in epidemic form when conditions are favorable for their spread.
- Epidemics are disasters by themselves but these can emerge in the aftermath of other disasters as well.
- In the recent past, two epidemics, viz., plague and dengue inflicted the Indian population very badly at Surat and Delhi, respectively. However, these occurred by themselves and were not the result of any other natural disaster.
The Surat (Gujarat) Plague Epidemic -1994
- Plague is a disease known to mankind from ancient times. India has undoubtedly a long history, which is replete with plague epidemics and havoc caused by them. This recent outbreak of plague generated a tremendous concern in and outside the country.
- No other disease so amenable to prevention and control has generated such serious concern in contemporary times. If its present epidemiological picture is appropriately examined, it does not deserve the attention it received.
- The reason for its larger than life size attention in the media in the country and outside, and the reason for the controversies which plagued this plague outbreak are possibly due to an inappropriate perception of the changing epidemiology of plague in modern era, when we have powerful management and diagnostic tools to contain the disease.
- This outbreak occurred in Surat on 1911 September, 1994.
- Following the sudden increase in the number of admitted cases with acute onset of fever, chest pain, cough, hemoptysis and deaths between 19th and 20th September, 1994 in different city hospitals, a sense of deep concern arose.
- As no history of rat fall could be elicited and typical bubonic cases were not seen, primary pneumonic plague outbreak was considered a possibility.
- The clinical presentation and the course of the disease pointed towards the pneumonic plague.
- Though stray cases were reported from other parts of the city, the major concentration of the reported cases came from the two adjacent localities of Ved Road and Katargam where the population were by and large Maharashtrians, the sanitation was very poor and the localities were highly congested slums.
- Furthermore, these areas are situated adjacent to river Tapti which was flooded between 7th and 9th September, 1994 due to heavy rains.
- About five lakh cusecs of water was released from the Ukai reservoir which led to the heavy water logging of the area.
- When the flood water started receding on 14th and 1511 September, 1994, the people of the localities started cleaning the areas and perhaps many of them handled dead wild rodents and animals.
- The Ganapati festival was observed with pomp and grandeur on 18fl1 September, 1994, when a large procession passed through the area and thereby getting infected probably.
- While the first patients were hospitalized on September 19, the panic was so great that by September 29, about 2 lakh persons (one-third of the population) had fled the city. During the period of the outbreak, 52 deaths were recorded from Surat city of which majority occurred before 25th September, 1994.
- A total of 1088 cases were suspected, about 146 were presumptive cases and 52 deaths due to plague took place during the period from 19th September, 1994 giving an overall case fatality rate of 4.8%.
- A study was carried out in Surat city during 8-19 November, 1994. Several identifiable risk factors were studied like occupation of the people, their visits outside Surat during the incubation period, exposure to a case, participation in the Ganapati procession festival, participation in cleaning operation, any associated illness, consumption of antibiotic, which could be accountable for the sporadic spread of the epidemic.
- The surprising thing was that the National Capital Delhi was also hit by the plague soon thereafter, although located faraway at about 1000 km. from Surat.
Control Measures
- Apart from identifying the patients and providing them proper medical treatment and care, a massive cleaning and sanitizing operation was conducted by the Municipal Corporation of Surat under the inspiring guidance of its Chief Executive whose efforts at cleaning up the city and thereby protecting it from epidemics were lauded nationally and internationally.
Dengue Epidemic in Delhi – 1996
- Dengue epidemic struck the Capital from mid-August to end-November, 1996, with Dengue Haemorrhagic Fever (DHF) and Dengue Shock Syndrome (DSS), the worst ever in India’s history. The virus, viz., Type II Dengue was identified as the causative agent in a number of clinical sanipies.
- There were in all about 10,000 cases with nearly 400 deaths as reported from all parts of the city.
- The following reasons were identified for the dramatic emergence in India of Dengue/DHF as a major public health problem:
- Ineffective Mosquito Control Programmes
- Major demographic and social changes, the most important being uncontrolled urbanization, excessive population growth and urban decay characterised by substandard housing and inadequate water and waste disposal systems; and
- Inadequate medical and health services.
- Dengue fever is caused by the bite of a mosquito known as Aedes Aegypti which profusely breeds in coolers, storage tanks, earthen pots and other receptacles with rainwater or stored clean water.
- There are a large number of other possible breeding places of Aedes Aegypti, viz., flower vases, neglected cups of jugs, household collection of water, neglected features of buildings, uncovered cisterns, wells, roof gutters, cracks in the masonry, traps of drains, flush tanks, ant traps, water receptacles of various kinds, rain filled empty cans or food tins, leaking water supply, water meters, sluice water chambers, water for birds, broken bottles, garden tanks, tree chambers, tree holes, fountains, troughs, a variety of dumps for engineering goods, trees, scraps and many more.
Control Measures
- Following the report of six deaths due to dengue at the All India Institute of Medical Sciences in The Times of India on September 13th 1996, the Municipal Corporation of Delhi (MCD) deputed two senior officers from the Antimalaria Department to collect the details.
- Containment measures were immediately taken in the localities from where these cases were reported.
- By September 14, 1996, the total number of cases admitted as DHF in Delhi was II.
- The MCD and the New Delhi Municipal Committee (NDMC) took the following measures:
- House to house survey for detection of vector breeding sources
- Intensification of anti-larval operation
- Focal spray with pyrethrum extract
- Intensification of health education Activities
- Public notice by way of newspapers to educate the people regarding dengue and to control the domestic breeding of mosquitoes was done.
- Likewise equipment like spray pumps, fogging machines were put in operation in large numbers.
- Control room for monitoring the situation and distribution of pyrethum solution to the NGOs was also taken-up.
- In the year 2001, dengue again seemed to appear in Delhi and a few cases were reported in October.
- Timely campaign against breeding of mosquitoes by public education and public health measures ensured that the disease did not attain epidemic status.
LESSONS LEARNT
Plague
- The diseases of the past can make their resurgence if favorable environment conditions are present. Efforts to prevent the resurgence of such deadly diseases have to be made by way of good sanitary conditions, hygiene and cleanliness.
- The decaying material including dead animals in the unsanitary conditions that usually prevails after the occurrence of destructive natural disaster situations such as earthquakes result in the spread of diseases/ epidemics as was seen in the case of the Latur earthquake of 1993.
- People living in poor sanitary conditions, congested slums and overcrowded localities are more prone to communicable diseases like plague.
- Migratory population and people participating in crowded functions during festivals and processions create conditions conducive for the spread of such diseases.
- Surveillance and monitoring programme for the diseases like plague are lacking at present. For want of required data/information on various causative factors, these epidemics cannot be forecast, thus further deterring timely preventive measures.
- Public needs to be educated about the signs and symptoms of likely diseases so as to enable the early detection and preventive measures of such diseases.
Local health authorities have to keep a constant vigil on the epidemic prone areas.
Dengue Fever
- The outbreaks of dengue including dengue hemorrhagic fever (DHF)/dengue shock syndrome (DSS) can be anticipated through a system of surveillance and monitoring of Vector densities.
- A check on the spread of epidemics by means of adequate control and monitoring measures before and after the occurrence of epidemics has to be ensured.
- Breeding conditions and the vector around Delhi and in other parts of the country pose a constant threat of dengue in India. Desert coolers, water storage tanks and utensils, leaking water supplies, wells and fountains, rain water collections and water bodies, tyre dumps, junk cans, rain-soaked and uncleared garbage dumps, etc. provide excellent places for Aedes breeding.
- DHF has become endemic and would surface periodically because of the very high vector breeding. The only practical approach to avoid future epidemics lies in preventive vector control with main reliance on source reduction and sanitation.
- Extensive training programme to update their knowledge and skills in this area is essential for health workers.
- We must accept and face the reality that dengue can surface again and to prevent future outbreaks, especially in the absence of any specific antiviral treatment or vaccine, sustained preventive community measures is the only key to success. Public education in this regard is very essential.
bacteria
The types of bacteria prevalent in an environment are determined by several factors. However, bacteria are found in every habitable place on earth. They survive in soil, rocks, oceans, volcanoes, and even arctic snow. Some have been found living in or on other organisms including plants, animals, and humans. The common types of bacteria found in buildings are not harmful when in low numbers. However, just like with mold, elevated levels of bacteria particularly the gram negative type are potentially a health hazard.
Some types of bacteria in buildings are brought in with occupants and with outdoor air. Others are human-gut-associated bacteria such as Lactobacillus, Staphylococcus and Clostridium. These types of bacteria are most common in bathroom environment. Research has shown that the types of bacteria in a building are also influenced by the type of ventilation, i.e., mechanically or naturally ventilated. For example, naturally ventilated buildings are associated with more plant- and soil-associated bacteria while mechanically ventilated buildings are likely to be dominated by human-associated bacteria.
Virus
Virus, an infectious agent of small size and simple composition that can multiply only in living cells of animals, plants, or bacteria. The name is from a Latin word meaning “slimy liquid” or “poison.”
The earliest indications of the biological nature of viruses came from studies in 1892 by the Russian scientist Dmitry I. Ivanovsky and in 1898 by the Dutch scientist Martinus W. Beijerinck. Beijerinck first surmised that the virus under study was a new kind of infectious agent, which he designated contagium vivum fluidum, meaning that it was a live, reproducing organism that differed from other organisms. Both of these investigators found that a disease of tobacco plants could be transmitted by an agent, later called tobacco mosaic virus, passing through a minute filter that would not allow the passage of bacteria. This virus and those subsequently isolated would not grow on an artificial medium and were not visible under the light microscope. In independent studies in 1915 by the British investigator Frederick W. Twort and in 1917 by the French Canadian scientist Félix H. d’Hérelle, lesions in cultures of bacteria were discovered and attributed to an agent called bacteriophage (“eater of bacteria”), now known to be viruses that specifically infect bacteria.
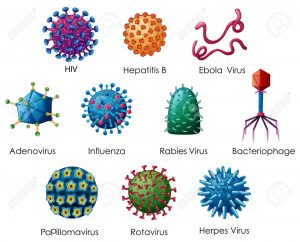
The unique nature of these organisms meant that new methods and alternative models had to be developed to study and classify them. The study of viruses confined exclusively or largely to humans, however, posed the formidable problem of finding a susceptible animal host. In 1933 the British investigators Wilson Smith, Christopher H. Andrewes, and Patrick P. Laidlaw were able to transmit influenza to ferrets, and the influenza virus was subsequently adapted to mice. In 1941 the American scientist George K. Hirst found that influenza virus grown in tissues of the chicken embryo could be detected by its capacity to agglutinate (draw together) red blood cells.
A significant advance was made by the American scientists John Enders, Thomas Weller, and Frederick Robbins, who in 1949 developed the technique of culturing cells on glass surfaces; cells could then be infected with the viruses that cause polio (poliovirus) and other diseases. (Until this time, the poliovirus could be grown only in the brains of chimpanzees or the spinal cords of monkeys.) Culturing cells on glass surfaces opened the way for diseases caused by viruses to be identified by their effects on cells (cytopathogenic effect) and by the presence of antibodies to them in the blood. Cell culture then led to the development and production of vaccines (preparations used to elicit immunity against a disease) such as the poliovirus vaccine.
Scientists were soon able to detect the number of bacterial viruses in a culture vessel by measuring their ability to break apart (lyse) adjoining bacteria in an area of bacteria (lawn) overlaid with an inert gelatinous substance called agar—viral action that resulted in a clearing, or “plaque.” The American scientist Renato Dulbecco in 1952 applied this technique to measuring the number of animal viruses that could produce plaques in layers of adjoining animal cells overlaid with agar. In the 1940s the development of the electron microscope permitted individual virus particles to be seen for the first time, leading to the classification of viruses and giving insight into their structure.
Advancements that have been made in chemistry, physics, and molecular biology since the 1960s have revolutionized the study of viruses. For example, electrophoresis on gel substrates gave a deeper understanding of the protein and nucleic acid composition of viruses. More-sophisticated immunologic procedures, including the use of monoclonal antibodies directed to specific antigenic sites on proteins, gave a better insight into the structure and function of viral proteins. The progress made in the physics of crystals that could be studied by X-ray diffraction provided the high resolution required to discover the basic structure of minute viruses. Applications of new knowledge about cell biology and biochemistry helped to determine how viruses use their host cells for synthesizing viral nucleic acids and proteins.
Logic originally dictated that viruses be identified on the basis of the host they infect. This is justified in many cases but not in others, and the host range and distribution of viruses are only one criterion for their classification. It is still traditional to divide viruses into three categories: those that infect animals, plants, or bacteria.
Virtually all plant viruses are transmitted by insects or other organisms (vectors) that feed on plants. The hosts of animal viruses vary from protozoans (single-celled animal organisms) to humans. Many viruses infect either invertebrate animals or vertebrates, and some infect both. Certain viruses that cause serious diseases of animals and humans are carried by arthropods. These vector-borne viruses multiply in both the invertebrate vector and the vertebrate host.
Certain viruses are limited in their host range to the various orders of vertebrates. Some viruses appear to be adapted for growth only in ectothermic vertebrates (animals commonly referred to as cold-blooded, such as fishes and reptiles), possibly because they can reproduce only at low temperatures. Other viruses are limited in their host range to endothermic vertebrates (animals commonly referred to as warm-blooded, such as mammals).
Fungi
fungi, any of about 99,000 known species of organisms of the kingdom Fungi, which includes the yeasts, rusts, smuts, mildews, molds, and mushrooms. There are also many funguslike organisms, including slime molds and oomycetes (water molds), that do not belong to kingdom Fungi but are often called fungi. Many of these funguslike organisms are included in the kingdom Chromista. Fungi are among the most widely distributed organisms on Earth and are of great environmental and medical importance. Many fungi are free-living in soil or water; others form parasitic or symbiotic relationships with plants or animals.
Fungi are eukaryotic organisms; i.e., their cells contain membrane-bound organelles and clearly defined nuclei. Historically, fungi were included in the plant kingdom; however, because fungi lack chlorophyll and are distinguished by unique structural and physiological features (i.e., components of the cell wall and cell membrane), they have been separated from plants. In addition, fungi are clearly distinguished from all other living organisms, including animals, by their principal modes of vegetative growth and nutrient intake. Fungi grow from the tips of filaments (hyphae) that make up the bodies of the organisms (mycelia), and they digest organic matter externally before absorbing it into their mycelia.
While mushrooms and toadstools (poisonous mushrooms) are by no means the most numerous or economically significant fungi, they are the most easily recognized. The Latin word for mushroom, fungus (plural fungi), has come to stand for the whole group. Similarly, the study of fungi is known as mycology—a broad application of the Greek word for mushroom, mykēs. Fungi other than mushrooms are sometimes collectively called molds, although this term is better restricted to fungi of the sort represented by bread mold. (For information about slime molds, which exhibit features of both the animal and the fungal worlds, see protist.)
Size range
The mushrooms, because of their size, are easily seen in fields and forests and consequently were the only fungi known before the invention of the microscope in the 17th century. The microscope made it possible to recognize and identify the great variety of fungal species living on dead or live organic matter. The part of a fungus that is generally visible is the fruiting body, or sporophore. Sporophores vary greatly in size, shape, colour, and longevity. Some are microscopic and completely invisible to the unaided eye; others are no larger than a pin head; still others are gigantic structures. Among the largest sporophores are those of mushrooms, bracket fungi, and puffballs. Some mushrooms reach a diameter of 20 to 25 cm (8 to 10 inches) and a height of 25 to 30 cm (10 to 12 inches). Bracket, or shelf, fungi can reach 40 cm (16 inches) or more in diameter. A specimen of the bracket fungus Fomitiporia ellipsoidea discovered in 2010 on Hainan Island in southern China had a fruiting body measuring 10.8 metres (35.4 feet) in length and 82–88 cm (2.7–2.9 feet) in width. It may have held some 450 million spores and weighed an estimated 400–500 kg (882–1,102 pounds), at the time making it the largest fungal fruiting body ever documented. Puffballs also can grow to impressive sizes. The largest puffballs on record measured 150 cm (5 feet) in diameter. The number of spores within such giants reaches several trillion.
Harmfull fungi
Many pathogenic fungi are parasitic in humans and are known to cause diseases of humans and other animals. In humans, parasitic fungi most commonly enter the body through a wound in the epidermis (skin). Such wounds may be insect punctures or accidentally inflicted scratches, cuts, or bruises. One example of a fungus that causes disease in humans is Claviceps purpurea, the cause of ergotism (also known as St. Anthony’s fire), a disease that was prevalent in northern Europe in the Middle Ages, particularly in regions of high rye-bread consumption. The wind carries the fungal spores of ergot to the flowers of the rye, where the spores germinate, infect and destroy the ovaries of the plant, and replace them with masses of microscopic threads cemented together into a hard fungal structure shaped like a rye kernel but considerably larger and darker. This structure, called an ergot, contains a number of poisonous organic compounds called alkaloids. A mature head of rye may carry several ergots in addition to noninfected kernels. When the grain is harvested, much of the ergot falls to the ground, but some remains on the plants and is mixed with the grain. Although modern grain-cleaning and milling methods have practically eliminated the disease, the contaminated flour may end up in bread and other food products if the ergot is not removed before milling. In addition, the ergot that falls to the ground may be consumed by cattle turned out to graze in rye fields after harvest. Cattle that consume enough ergot may suffer abortion of fetuses or death. In the spring, when the rye is in bloom, the ergot remaining on the ground produces tiny, black, mushroom-shaped bodies that expel large numbers of spores, thus starting a new series of infections.
Other human diseases caused by fungi include athlete’s foot, ringworm, aspergillosis, histoplasmosis, and coccidioidomycosis. The yeast Candida albicans, a normal inhabitant of the human mouth, throat, colon, and reproductive organs, does not cause disease when it is in ecological balance with other microbes of the digestive system. However, disease, age, and hormonal changes can cause C. albicans to grow in a manner that cannot be controlled by the body’s defense systems, resulting in candidiasis (called thrush when affecting the mouth). Candidiasis is characterized by symptoms ranging from irritating inflamed patches on the skin or raised white patches on the tongue to life-threatening invasive infection that damages the lining of the heart or brain. Improved diagnosis and increased international travel, the latter of which has facilitated the spread of tropical pathogenic fungi, have resulted in an increased incidence of fungal disease in humans. In addition, drug therapies used to manage the immune system in transplant and cancer patients weaken the body’s defenses against fungal pathogens. Patients infected with human immunodeficiency virus (HIV), the causative agent of acquired immunodeficiency syndrome (AIDS), have similarly weakened immune defenses against fungi, and many AIDS-related deaths are caused by fungal infections (especially infection with Aspergillus fumigatus).
APPSC GROUP 1 Notes brings Prelims and Mains programs for APPSC GROUP 1 Prelims and APPSC GROUP 1 Mains Exam preparation. Various Programs initiated by APPSC GROUP 1 Notes are as follows:-- APPSC GROUP 1 Mains Tests and Notes Program
- APPSC GROUP 1 Prelims Exam - Test Series and Notes Program
- APPSC GROUP 1 Prelims and Mains Tests Series and Notes Program
- APPSC GROUP 1 Detailed Complete Prelims Notes